Cvs Caremark Prior Authorization Form For Remicade . Web by signing above, i hereby authorize cvs specialty pharmacy and/or its affiliate pharmacies to complete and submit prior. Has the patient been receiving the requested drug within the last 120 days? Web this patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. Web this patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. Web electronic prior authorization information. Web covermymeds is cvs caremark prior authorization forms’s preferred method for receiving epa requests. Web submission of the following information is necessary to initiate the prior authorization review: Has the requested drug been. Web this policy informs prescribers of preferred products and provides an exception.
from www.sampletemplates.com
Web submission of the following information is necessary to initiate the prior authorization review: Web this patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. Has the requested drug been. Web covermymeds is cvs caremark prior authorization forms’s preferred method for receiving epa requests. Has the patient been receiving the requested drug within the last 120 days? Web electronic prior authorization information. Web by signing above, i hereby authorize cvs specialty pharmacy and/or its affiliate pharmacies to complete and submit prior. Web this policy informs prescribers of preferred products and provides an exception. Web this patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered.
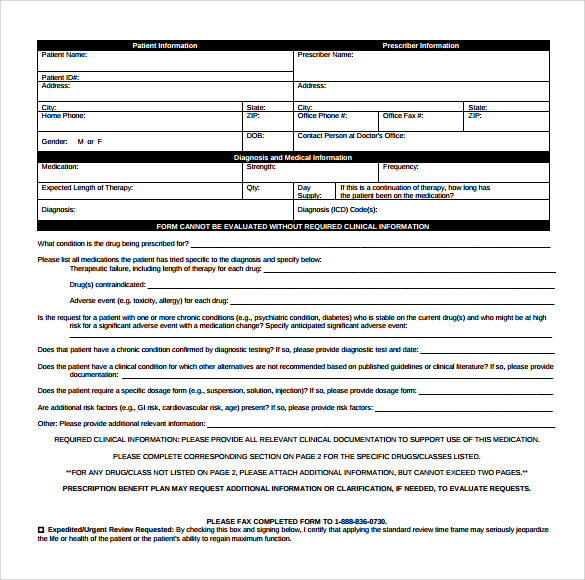
9+ Sample Caremark Prior Authorization Forms Sample Templates
Cvs Caremark Prior Authorization Form For Remicade Web electronic prior authorization information. Web covermymeds is cvs caremark prior authorization forms’s preferred method for receiving epa requests. Has the patient been receiving the requested drug within the last 120 days? Web this policy informs prescribers of preferred products and provides an exception. Web this patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. Web electronic prior authorization information. Web by signing above, i hereby authorize cvs specialty pharmacy and/or its affiliate pharmacies to complete and submit prior. Web this patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. Web submission of the following information is necessary to initiate the prior authorization review: Has the requested drug been.
From exobjyvlx.blob.core.windows.net
Cvs Caremark Prior Auth Forms Pdf at Milly Hicks blog Cvs Caremark Prior Authorization Form For Remicade Web this patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. Web this patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. Has the requested drug been. Web covermymeds is cvs caremark prior authorization forms’s preferred method for receiving epa requests. Has the patient. Cvs Caremark Prior Authorization Form For Remicade.
From moussyusa.com
Template Caremark Prior Authorization Form Mous Syusa Cvs Caremark Prior Authorization Form For Remicade Web this policy informs prescribers of preferred products and provides an exception. Has the patient been receiving the requested drug within the last 120 days? Web electronic prior authorization information. Web this patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. Web covermymeds is cvs caremark prior authorization forms’s preferred method for. Cvs Caremark Prior Authorization Form For Remicade.
From www.reddit.com
Second Prior Authorization APPROVED!!! CVS Caremark r/Zepbound Cvs Caremark Prior Authorization Form For Remicade Web submission of the following information is necessary to initiate the prior authorization review: Web this patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. Web this policy informs prescribers of preferred products and provides an exception. Web electronic prior authorization information. Web this patient’s benefit plan requires prior authorization for certain. Cvs Caremark Prior Authorization Form For Remicade.
From www.sampletemplates.com
FREE 8+ Sample Caremark Prior Authorization Forms in PDF Cvs Caremark Prior Authorization Form For Remicade Web covermymeds is cvs caremark prior authorization forms’s preferred method for receiving epa requests. Web this patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. Web electronic prior authorization information. Web this patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. Has the patient. Cvs Caremark Prior Authorization Form For Remicade.
From www.pdffiller.com
Cigna Remicade Prior Authorization Form Fill Online, Printable Cvs Caremark Prior Authorization Form For Remicade Web this policy informs prescribers of preferred products and provides an exception. Has the requested drug been. Web this patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. Web this patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. Web covermymeds is cvs caremark. Cvs Caremark Prior Authorization Form For Remicade.
From eforms.com
Free CVS/Caremark Prior (Rx) Authorization Form PDF eForms Cvs Caremark Prior Authorization Form For Remicade Web submission of the following information is necessary to initiate the prior authorization review: Web by signing above, i hereby authorize cvs specialty pharmacy and/or its affiliate pharmacies to complete and submit prior. Web this policy informs prescribers of preferred products and provides an exception. Web this patient’s benefit plan requires prior authorization for certain medications in order for the. Cvs Caremark Prior Authorization Form For Remicade.
From www.signnow.com
Cvs Caremark Appeal PDF 20032024 Form Fill Out and Sign Printable Cvs Caremark Prior Authorization Form For Remicade Web electronic prior authorization information. Web this patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. Web by signing above, i hereby authorize cvs specialty pharmacy and/or its affiliate pharmacies to complete and submit prior. Web covermymeds is cvs caremark prior authorization forms’s preferred method for receiving epa requests. Web this policy. Cvs Caremark Prior Authorization Form For Remicade.
From www.formsbank.com
Top 7 Caremark Prior Authorization Form Templates free to download in Cvs Caremark Prior Authorization Form For Remicade Has the requested drug been. Web submission of the following information is necessary to initiate the prior authorization review: Has the patient been receiving the requested drug within the last 120 days? Web this policy informs prescribers of preferred products and provides an exception. Web electronic prior authorization information. Web this patient’s benefit plan requires prior authorization for certain medications. Cvs Caremark Prior Authorization Form For Remicade.
From www.sampletemplates.com
9+ Sample Caremark Prior Authorization Forms Sample Templates Cvs Caremark Prior Authorization Form For Remicade Web this policy informs prescribers of preferred products and provides an exception. Has the patient been receiving the requested drug within the last 120 days? Web covermymeds is cvs caremark prior authorization forms’s preferred method for receiving epa requests. Web by signing above, i hereby authorize cvs specialty pharmacy and/or its affiliate pharmacies to complete and submit prior. Web this. Cvs Caremark Prior Authorization Form For Remicade.
From www.sampletemplates.com
FREE 8+ Sample Caremark Prior Authorization Forms in PDF Cvs Caremark Prior Authorization Form For Remicade Web this patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. Web electronic prior authorization information. Web submission of the following information is necessary to initiate the prior authorization review: Has the requested drug been. Web covermymeds is cvs caremark prior authorization forms’s preferred method for receiving epa requests. Web this patient’s. Cvs Caremark Prior Authorization Form For Remicade.
From cvs-prior-auth-form.pdffiller.com
Cvs Caremark Prior Authorization Form Fill Online, Printable Cvs Caremark Prior Authorization Form For Remicade Has the patient been receiving the requested drug within the last 120 days? Web covermymeds is cvs caremark prior authorization forms’s preferred method for receiving epa requests. Web this patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. Web this policy informs prescribers of preferred products and provides an exception. Web this. Cvs Caremark Prior Authorization Form For Remicade.
From www.authorizationform.net
Cvs Caremark Wegovy Prior Authorization Form Cvs Caremark Prior Authorization Form For Remicade Web electronic prior authorization information. Web submission of the following information is necessary to initiate the prior authorization review: Has the patient been receiving the requested drug within the last 120 days? Web this policy informs prescribers of preferred products and provides an exception. Has the requested drug been. Web this patient’s benefit plan requires prior authorization for certain medications. Cvs Caremark Prior Authorization Form For Remicade.
From www.sampletemplates.com
FREE 8+ Sample Caremark Prior Authorization Forms in PDF Cvs Caremark Prior Authorization Form For Remicade Web this patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. Web covermymeds is cvs caremark prior authorization forms’s preferred method for receiving epa requests. Web submission of the following information is necessary to initiate the prior authorization review: Web electronic prior authorization information. Web by signing above, i hereby authorize cvs. Cvs Caremark Prior Authorization Form For Remicade.
From moussyusa.com
Template Caremark Prior Authorization Form Mous Syusa Cvs Caremark Prior Authorization Form For Remicade Has the patient been receiving the requested drug within the last 120 days? Web this patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. Web this patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. Has the requested drug been. Web covermymeds is cvs. Cvs Caremark Prior Authorization Form For Remicade.
From www.uslegalforms.com
Cvs Caremark Prescription Form 20202022 Fill and Sign Printable Cvs Caremark Prior Authorization Form For Remicade Web this patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. Has the patient been receiving the requested drug within the last 120 days? Web electronic prior authorization information. Web submission of the following information is necessary to initiate the prior authorization review: Has the requested drug been. Web this policy informs. Cvs Caremark Prior Authorization Form For Remicade.
From exoikgzme.blob.core.windows.net
Cvs Specialty Refill Form at Oscar Gray blog Cvs Caremark Prior Authorization Form For Remicade Web by signing above, i hereby authorize cvs specialty pharmacy and/or its affiliate pharmacies to complete and submit prior. Web this patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. Has the requested drug been. Web this patient’s benefit plan requires prior authorization for certain medications in order for the drug to. Cvs Caremark Prior Authorization Form For Remicade.
From www.formsbank.com
Top 20 Cvs Caremark Forms And Templates free to download in PDF format Cvs Caremark Prior Authorization Form For Remicade Web this patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. Web this patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. Web this policy informs prescribers of preferred products and provides an exception. Web submission of the following information is necessary to initiate. Cvs Caremark Prior Authorization Form For Remicade.
From moussyusa.com
Template Caremark Prior Authorization Form Mous Syusa Cvs Caremark Prior Authorization Form For Remicade Has the patient been receiving the requested drug within the last 120 days? Has the requested drug been. Web covermymeds is cvs caremark prior authorization forms’s preferred method for receiving epa requests. Web this policy informs prescribers of preferred products and provides an exception. Web this patient’s benefit plan requires prior authorization for certain medications in order for the drug. Cvs Caremark Prior Authorization Form For Remicade.